Introduction: A New COVID-19 Variant Emerges
As the world enters its fifth year of living with COVID-19, a new variant—NB.1.8.1, unofficially nicknamed “Nimbus”—is quietly making its way across continents. First detected in early 2025, this Omicron sub-lineage has now been confirmed in over 20 countries, including the United States, United Kingdom, China, Australia, Bangladesh, and several others in Asia and Europe. Unlike the dramatic surges of previous waves, Nimbus is spreading with little fanfare, often going unnoticed due to its mild or atypical symptoms and a general decline in public vigilance. Yet, health authorities and experts warn that its silent spread could pose unique challenges for global public health.
- Introduction: A New COVID-19 Variant Emerges
- What Is NB.1.8.1 ‘Nimbus’?
- How Is Nimbus Different from Previous Variants?
- Symptoms: What Does Infection with Nimbus Feel Like?
- Where Is Nimbus Spreading?
- Why Is Detection So Difficult?
- How Dangerous Is Nimbus? Severity and Long-Term Risks
- Vaccine Effectiveness and Changing Guidelines
- Public Health Response: What Are Authorities Doing?
- What Should Individuals Do?
- Broader Implications: The Future of COVID-19 Surveillance
- In Summary
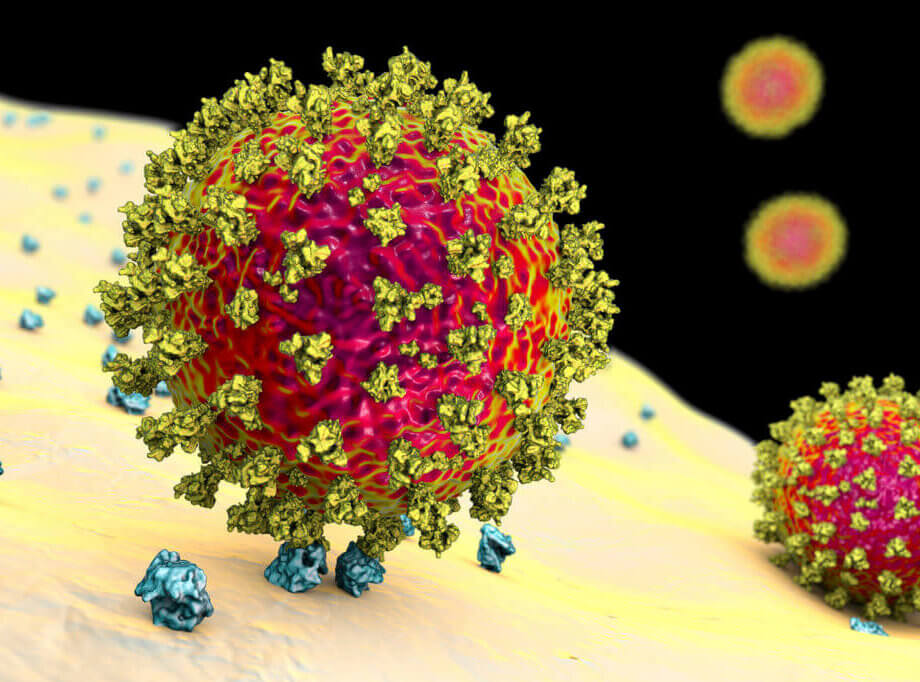
What Is NB.1.8.1 ‘Nimbus’?
NB.1.8.1 is a descendant of the Omicron variant, itself a highly mutated and transmissible branch of the SARS-CoV-2 virus. Like its predecessors, Nimbus has accumulated several mutations in its spike protein—the part of the virus that allows it to enter human cells. These changes may make it more transmissible and help it partially evade immunity from previous infections or vaccinations. The World Health Organization (WHO) has classified NB.1.8.1 as a “variant under monitoring,” meaning it is spreading rapidly enough to warrant close observation, though it has not yet shown increased severity compared to other variants.
Genetic sequencing data from GISAID, a global virus database, shows that NB.1.8.1 was first identified in travelers from East Asia and Europe in January 2025. Since then, it has become the dominant strain in China and Hong Kong, and is responsible for a growing share of cases in the U.S., India, Singapore, Thailand, and beyond. In the U.S., the Centers for Disease Control and Prevention (CDC) estimates that NB.1.8.1 now accounts for about 37% of new COVID-19 cases, rivaling the previously dominant LP.8.1 variant.
How Is Nimbus Different from Previous Variants?
While NB.1.8.1 shares many characteristics with other Omicron subvariants, it stands out for several reasons:
- Increased Transmissibility: Laboratory studies suggest that NB.1.8.1 binds more efficiently to the human ACE2 receptor, the gateway for the virus into cells. This could make it easier to spread from person to person, even among those with some level of immunity.
- Immune Evasion: Some of Nimbus’s mutations may help it partially escape antibodies generated by previous infections or vaccinations. However, current evidence indicates that vaccines still provide strong protection against severe illness and hospitalization.
- Silent Spread: Perhaps the most concerning feature is how quietly Nimbus spreads. Many infected individuals experience only mild symptoms—or none at all—making detection and containment more difficult.
Dr. Chun Tang, a general practitioner in the UK, explains:
“NB.1.8.1 isn’t too different from the Omicron variant, but it does have some tweaks to its spike protein, which might make it spread a bit more easily or slip past some of our existing immunity. That said, early signs suggest it doesn’t seem to cause more serious illness, but of course, we’re still learning more about it.”
Symptoms: What Does Infection with Nimbus Feel Like?
The symptoms of NB.1.8.1 are generally similar to those of other Omicron variants, but with some notable differences. The most commonly reported symptoms include:
- Severe sore throat (often described as “razor blade throat”)
- Fatigue
- Mild cough
- Congestion or runny nose
- Fever or chills
- Muscle aches
- Headache
- Nausea and, less commonly, diarrhea
- Loss of taste or smell (less frequent than in earlier variants)
Many people infected with Nimbus report only mild symptoms, such as a slight sore throat or feeling unusually tired. Some experience gastrointestinal symptoms, while others may not realize they are infected at all. This makes it easy for the virus to circulate undetected, especially as routine testing and public awareness have declined.
Dr. T. Ryan Gregory, a Canadian evolutionary biologist who coined the nickname “Nimbus,” notes:
“We learned from Omicron that high transmissibility can cause as much damage as high per infection virulence, and at this point it is not just acute severity that is of concern, but longer-term impacts of repeated infection.”
Where Is Nimbus Spreading?
NB.1.8.1 has been detected in at least 22 countries, with significant activity in:
- China and Hong Kong: Now the dominant strain, contributing to spikes in emergency room visits and hospitalizations.
- United States: Detected in at least 14 states, including California, New York, Ohio, Rhode Island, Virginia, and Washington. It now accounts for over a third of new cases.
- India: Over 1,000 active cases reported as of late May 2025, with notable clusters in Delhi and Tamil Nadu.
- Singapore and Thailand: Both countries have seen significant surges, with Singapore’s weekly cases rising from 11,100 to 14,200 in early May, and Thailand’s cases jumping from 6,000 to over 33,000 in a matter of days.
- Bangladesh: The Directorate General of Health Services (DGHS) has issued a nationwide alert after confirming the variant’s presence.
- Europe and Australia: Cases have been reported in the UK, France, the Netherlands, Spain, and Australia, though at lower levels than in Asia.
Due to reduced testing and sequencing, the true number of cases is likely much higher than reported. Wastewater surveillance and airport screening programs have become key tools for tracking the variant’s spread.
Why Is Detection So Difficult?
Unlike earlier waves of COVID-19, the spread of NB.1.8.1 is not accompanied by dramatic surges in hospitalizations or mass testing lines. Instead, its mild or asymptomatic presentation means many cases go undetected. Public health experts warn that this could allow the variant to circulate widely before authorities realize the extent of its spread.
Dr. Rajendram Rajnarayanan, a virologist at the New York Institute of Technology, emphasizes the challenge:
“We haven’t seen a big surge in emergency departments due to COVID-related conditions and respiratory things in this term yet. We have to wait and watch.”
With fewer people seeking tests and many countries scaling back surveillance, the risk is that outbreaks could grow silently, especially in vulnerable populations.
How Dangerous Is Nimbus? Severity and Long-Term Risks
So far, there is no evidence that NB.1.8.1 causes more severe illness or higher rates of hospitalization and death than previous Omicron variants. The WHO, CDC, and other health agencies have all assessed the global risk as “low” at this time. Most people experience mild symptoms, and current vaccines remain effective at preventing severe disease.
However, experts caution that high transmissibility can still have significant public health impacts. Even if only a small percentage of cases result in severe illness, a large number of infections can still strain healthcare systems, especially if vulnerable groups are affected. There is also concern about the long-term effects of repeated COVID-19 infections, including the risk of “long COVID,” which can cause persistent symptoms for months or years.
Dr. T. Ryan Gregory highlights the importance of continued vigilance:
“It is not just about protecting people today but also protecting them from any other variant in the future.”
Vaccine Effectiveness and Changing Guidelines
Current COVID-19 vaccines, including the latest boosters, are expected to remain effective against NB.1.8.1, particularly in preventing severe illness and hospitalization. The variant’s mutations may allow it to partially evade antibodies, but not to the extent that would render vaccines ineffective.
However, recent changes in vaccination guidelines in the U.S. and other countries have raised concerns about access and coverage. The CDC and FDA have updated their recommendations, now limiting routine COVID-19 vaccination to adults 65 and older and people ages 12-64 with underlying health conditions. Routine vaccination is no longer recommended for healthy children and pregnant women, though many medical professionals disagree with this change. These policy shifts may make it harder for some people to access vaccines, especially if insurance coverage is affected.
Dr. Albert Ko, professor at Yale School of Public Health, advises:
“Those in high-risk groups should consider getting the vaccine now if they haven’t been vaccinated in the last six months and consider receiving an updated vaccine for the upcoming winter season.”
Public Health Response: What Are Authorities Doing?
In response to the spread of NB.1.8.1, health authorities in affected countries have issued renewed guidance and alerts. The DGHS in Bangladesh, for example, has called for increased precautions at ports of entry, hospitals, and crowded public spaces. Healthcare workers are being reminded to prepare isolation facilities, use personal protective equipment (PPE), and screen travelers at airports and land borders.
The World Health Network and other organizations recommend the following measures to reduce transmission:
- Monitor local wastewater readings to assess COVID-19 levels in the community
- Wear high-quality masks (such as N95 respirators) in crowded or indoor settings
- Improve indoor air quality by increasing ventilation and using HEPA air purifiers
- Get tested if symptomatic or after known exposure
- Stay home and avoid in-person meetings if feeling unwell
- Stay up to date with COVID-19 vaccinations and boosters, especially for high-risk groups
Despite these recommendations, public vigilance has waned after years of pandemic fatigue. Many people have stopped wearing masks or seeking tests, and funding for surveillance and research has declined in some regions. Experts warn that this complacency could allow new variants like Nimbus to spread unchecked.
What Should Individuals Do?
While the overall risk from NB.1.8.1 remains low for most people, especially those who are vaccinated and healthy, it is important to remain cautious—particularly for those at higher risk of severe illness. The following steps can help protect yourself and others:
- Wear a mask in crowded or poorly ventilated spaces
- Wash hands regularly and practice good respiratory hygiene
- Stay home if you feel unwell, even with mild symptoms
- Get tested if you develop symptoms or have been exposed to someone with COVID-19
- Keep up to date with vaccine recommendations and boosters
- Consult your healthcare provider if you have questions about vaccination or symptoms
Broader Implications: The Future of COVID-19 Surveillance
The emergence of NB.1.8.1 highlights the ongoing evolution of SARS-CoV-2 and the need for continued vigilance. As the virus mutates, new variants will continue to arise, some of which may spread more easily or evade immunity. Reduced testing and surveillance make it harder to detect and respond to these changes in real time.
Experts stress the importance of maintaining robust public health infrastructure, including genomic surveillance, wastewater monitoring, and clear communication with the public. The experience with Nimbus serves as a reminder that the pandemic is not over, even if its most dramatic phases have passed.
As one health official in Bangladesh noted:
“This variant isn’t loud. That’s exactly why we need to listen.”
In Summary
- NB.1.8.1, or “Nimbus,” is a new Omicron subvariant spreading quietly across more than 20 countries.
- It is more transmissible than previous variants and can partially evade immunity, but does not appear to cause more severe illness.
- Symptoms are often mild or atypical, making detection and containment challenging.
- Current vaccines remain effective at preventing severe disease, though access and guidelines are changing in some countries.
- Public health authorities recommend renewed vigilance, including masking, testing, and vaccination, especially for high-risk groups.
- The silent spread of Nimbus underscores the need for ongoing surveillance and public awareness as the virus continues to evolve.