Why a simple fridge door ping could save a life
After a string of tragic discoveries involving older residents who died alone in their flats, Hong Kong officials are looking at simple household signals to check daily wellbeing. The Labour and Welfare Bureau is studying whether sensors that notice when a front door or a refrigerator door opens can serve as an early warning when routines suddenly stop. The idea is low cost and passive. It aims to support seniors who want to age at home while easing pressure on stretched care teams.
- Why a simple fridge door ping could save a life
- What fridge and door sensors can reveal
- Wearables and smart devices on trial
- Inside care homes of the future
- Public acceptance, privacy and consent
- How tech could link with social workers
- Costs and feasibility in practice
- Lessons from research and pilots
- Regional moves in the Greater Bay Area
- Risks, safeguards and governance
- What to Know
Hong Kong has one of the worlds longest life expectancies at about 85 years, and the share of residents aged 65 and above is rising fast. Community care has become a central plank of policy, since care home places are limited and most older adults prefer to stay in familiar neighbourhoods. Technology, often called gerontechnology, is moving from pilot projects to practical tools that connect families, social workers and clinics with those living alone.
Speaking on a radio programme, Labour and Welfare Secretary Chris Sun Yuk-han described how off the shelf devices might help with early detection and faster outreach.
‘We are currently exploring the use of wearable systems or other technologies that we have seen in the market. It is rather simple, for example, by detecting the opening and closing of your refrigerator door or the door of your flat to assess whether you are living a normal life or maybe experiencing some problems. In that case, we can try to contact you promptly.’
Officials say the aim is not intrusive surveillance. Instead, it is a light touch approach, combining a handful of routine signals with human follow up. If a fridge is not opened from morning to evening, or if no movement is recorded at a front door for a day when a person usually goes out to buy lunch, the system can flag a welfare check by a call centre, a neighbourhood team or family members.
What fridge and door sensors can reveal
Door and fridge sensors are simple contact or motion devices. They send a ping to a small hub at home, which relays status to a secure platform. No cameras or microphones are needed. The data point is binary, open or closed, yet it can paint a picture of daily rhythm, like breakfast, lunch and grocery runs. When that rhythm stalls, responders can look in quickly.
How an alert might work
A city run pilot could standardise a few rules and give clear opt in choices. A profile can be set with the seniors consent and with input from a case manager. Alerts can escalate in steps rather than triggering an ambulance on the first missed pattern.
- No fridge door opening within 12 hours during daytime triggers a call.
- No front door activity for 24 hours triggers a call, followed by a neighbour knock.
- Manual panic button press triggers emergency services.
- Battery running low prompts maintenance visit.
No pattern is perfect. A senior may nap longer than usual, eat out or spend a night with relatives. To reduce false calls, systems can include check in calls, two way voice prompts and quick ways to snooze alerts. The goal is a safety net that respects autonomy while catching genuine emergencies such as falls, strokes or sudden illness.
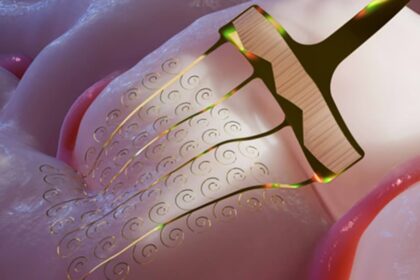
Wearables and smart devices on trial
Wearable devices are the other pillar under review. Smart watches and pendants designed for seniors track steps, heart rate and sleep, and can detect a hard fall using accelerometers. Many models include a one touch help button. Local integrators already provide cloud dashboards for care teams. In homes and centres, bed exit sensors and radar based fall detectors alert staff when someone gets up at night or falls in a bathroom.
Guardforce Hong Kong describes anti wandering solutions that watch exits and send alerts when a resident with dementia moves toward a stairwell or leaves a safe area. These systems range from simple wrist tags to facial recognition tied to existing cameras. Vendors argue that pairing wearables with fixed sensors offers broader coverage at modest cost, while keeping visual surveillance to a minimum.
Companies such as Fujitsu propose non invasive audio sensing that listens for coughing, heavy breathing or unusual loud sounds like a fall, then cross checks with motion sensors. Software routes alerts to a service centre that can speak with the resident over a speaker, call family, or dispatch help. Their companion kits pair with blood pressure cuffs and oximeters for remote vital sign checks that doctors can review between clinic visits.
Inside care homes of the future
A vast smart care complex now in planning shows where the sector is heading. The Pok Oi Hospital Tuen Mun Lam Tei project, created with the Hong Kong Applied Science and Technology Research Institute, aims to embed digital systems across daily care, from IoT sensors to robotics. When it opens, the facility plans to handle more than 1,400 residents and to serve as a model others can copy.
Project leaders say generative AI will sift real time health data to spot risk early, robots will assist with mobility and therapy, and environmental sensors will tune lighting and air quality. Energy management is part of the design to keep costs down without sacrificing comfort. The concept mirrors a shift worldwide, where care teams use data and automation to support better outcomes despite staff shortages.
Private sector investment is moving too. Hong Kong based service robotics firms are raising funds to expand telemedicine and elder care tools, while deploying helper robots in hospitals and care homes. Their pitch is simple. Machines handle routine tasks and triage, humans focus on personal care.
Public acceptance, privacy and consent
Any citywide use of home sensors needs clear consent rules and strict data protection. Hong Kong law under the Personal Data Privacy Ordinance sets baseline duties. Collection must be for a specific purpose, data must be kept to a minimum, stored safely and used only by authorised staff. Seniors and families need to know what is recorded, who sees it, and how long it is kept.
Many older adults welcome technology if it is useful and easy. Research with 306 Hong Kong residents aged 60 and above found that optimism and perceived usefulness drive willingness to try digital health tools. Higher eHealth literacy also softens worries and helps people judge value. The lesson for government is practical. Pair devices with training and simple instructions, and offer a hotline that can talk someone through a pairing or a reset.
Privacy by design can be baked in from the start. Fridge or door sensors do not capture images. Systems can anonymise routine telemetry and decrypt personal details only when an alert escalates. Access logs and audit trails can deter misuse. Public oversight, for example through an advisory panel with community leaders and carers, can help maintain trust.
How tech could link with social workers
There is no single agency that can check on every senior every day. Technology helps by routing alerts to the right team at the right time. A practical network could include district social welfare offices, non profit outreach teams, public housing estate staff and volunteer groups.
A typical escalation might look like this. A missed fridge pattern triggers a soft check by phone. If there is no answer, a neighbour or estate concierge knocks on the door. Persistent silence prompts a call to the family or a case manager. If a second device also looks abnormal, responders call emergency services for a welfare visit. Each step is logged with time and outcome.
Families often ask who pays and who monitors. City backed call centres can keep first line duties while families can also receive the same alerts on a phone app. That shared view reduces anxiety and keeps relatives in the loop, whether they live nearby or overseas.
Costs and feasibility in practice
Simple magnetic door sensors and a home gateway can cost only a few hundred Hong Kong dollars per household at scale. Wearable watches range widely, from basic fall detectors to cellular models with GPS. The larger cost is the monitoring service and the response network. Governments often pilot with a small cohort, then handle procurement to drive down unit prices.
A balanced package for a person living alone might include one door sensor, one fridge sensor, a wearable panic button, and an option to add a bed exit sensor. The monitoring platform should accept devices from multiple brands to avoid lock in. Procurement can require open standards and clear service level targets for response times and equipment upkeep.
Funding can align with existing community care vouchers and innovation funds, with priority for high risk households in aging districts. Care teams will still make home visits, but fewer checks will be blind. The mix of proactive sensing and scheduled visits stretches staff time and reaches more people.
Lessons from research and pilots
A pilot in Hong Kong that combined a small inertial sensor with a depth camera during standard balance tests showed promise. Forty four older adults used the system to run through timed up and go, sit to stand and standing balance tasks. Statistical models predicted scores that therapists use in clinics. Participants said the system was useful and easy to use. That kind of evidence supports wider rollouts for fall risk screening in the community.
Beyond clinics, many care providers already rely on bed exit alarms and radar fall detectors that do not need users to wear anything. Those tools can complement door and fridge sensors. If night movement is detected and the fridge shows activity at 2 a.m., the platform can suppress alarms that would otherwise call staff, reducing alarm fatigue.
Studies of technology adoption among older adults in Hong Kong highlight a recurring pattern. Perceived usefulness and ease of use shape attitudes, which then predict intention to use. Training boosts confidence. When family members encourage a new tool, take up rises. Programme design can build on this by including onboarding sessions with both seniors and their adult children.
Regional moves in the Greater Bay Area
Hong Kong is not working in isolation. Across the Greater Bay Area, policymakers and researchers are exploring cross border elderly care models and a broader silver economy. Universities and consulting groups have signed agreements to develop a smart ecosystem for older residents that joins finance, healthcare and technology.
Plans include shared platforms for secure data exchange, and trials of remote care using tools such as virtual reality and augmented reality for rehabilitation. The idea is to give seniors the option to access care closer to family or lower cost services without losing continuity of records. Progress across the region can also feed back into Hong Kong pilots and bring affordable devices to market faster.
Risks, safeguards and governance
Every monitoring system has trade offs. Over alerting can strain hotlines. Under alerting can miss a crisis. Battery failures and network outages must be planned for with back up checks. Policy should define who is responsible at each point of the chain so that no alert falls through gaps.
Seniors who dislike technology or fear stigma should never be forced to participate. Choice matters. Alternatives like regular check in calls or scheduled visits must remain. Equity also matters. If sensors are offered first to public housing residents in older districts, the city should be ready to scale to private flats and rural homes.
Open reporting can keep the public informed. Metrics such as alerts handled, response times, confirmed emergencies detected and false alarm rates can be published. Programme boards can include carers, nurses, social workers and patient advocates. That breadth helps keep priorities focused on dignity and safety, not just devices.
What to Know
- The government is testing door and fridge sensors and wearables to check daily wellbeing of seniors living alone.
- Fridge or door patterns that stop can trigger staged outreach, starting with a call and moving to a knock and a welfare visit.
- Wearables, bed exit sensors and radar fall detectors are already in use by local providers.
- A smart elderly care complex in Lam Tei plans to integrate AI, robotics and IoT across care operations by 2027.
- Research in Hong Kong finds older adults accept digital health tools when they are useful, easy and paired with training.
- Privacy safeguards under local law require clear consent, minimal data collection and strong security.
- Programs should link alerts to social workers, estate staff and families to speed checks without overburdening emergency services.
- Costs depend on scale, but basic sensor kits are relatively affordable compared with full time in person monitoring.